Introduction
Trauma during pregnancy is a major concern, and car accidents are unfortunately a leading cause. If a pregnant woman is involved in a car crash and rushed to the emergency room or trauma bay, prompt and accurate diagnosis is critical for both her health and the baby’s wellbeing. In these urgent situations, Computed Tomography (CT) scans often become a vital tool. While there’s understandable concern about radiation exposure during pregnancy, especially with procedures like a Bay Car Ct Scan, it’s crucial to understand that in trauma scenarios, the benefits of a CT scan often outweigh the risks. This article will explore why CT scans are essential in the initial assessment of pregnant trauma patients, particularly those involved in car accidents and brought to the trauma bay setting, addressing radiation concerns and outlining the best practices for imaging. The primary goal in these critical moments is always maternal stabilization, as this is the most direct path to a positive fetal outcome.
Understanding the Importance of CT Scans in the Trauma Bay for Pregnant Patients After Car Accidents
When a pregnant woman arrives in the trauma bay following a car accident, healthcare providers face a complex situation. Pregnancy brings about significant physiological and anatomical changes that can both increase the risk of specific injuries and make diagnosis more challenging. The growing uterus, while protecting the fetus, can also be a site of injury and can obscure other internal injuries. Rapid and accurate diagnosis is paramount to guide immediate treatment decisions.
For any trauma patient, including pregnant women, diagnostic imaging is indispensable. A bay car ct scan is often a cornerstone of this initial assessment, allowing doctors to quickly visualize internal injuries that might not be apparent through physical examination alone. Delaying or avoiding necessary CT scans due to radiation concerns can have serious consequences, potentially leading to missed diagnoses and delayed treatment, which can be detrimental to both mother and fetus. The decision to use CT scans in pregnant trauma patients is not taken lightly, but it is often a necessary step to ensure the best possible outcomes.
Radiation Concerns and Fetal Safety: Addressing Common Questions About Bay Car CT Scans
One of the primary concerns surrounding the use of a bay car ct scan in pregnant women is the exposure to ionizing radiation and its potential effects on the developing fetus. For decades, this concern has been at the forefront of discussions regarding imaging pregnant patients. It’s important to understand the facts about radiation exposure from CT scans and how advancements in technology and knowledge have changed our understanding of these risks.
Modern CT technology has significantly reduced radiation doses compared to older scanners. Innovations like improved detectors, faster scanning speeds, automated dose modulation, and advanced reconstruction techniques all contribute to minimizing radiation exposure during a bay car ct scan. Furthermore, our understanding of the biological effects of radiation has evolved, leading to refined guidelines and practices aimed at patient safety.
It’s crucial to differentiate between deterministic and stochastic effects of radiation. Deterministic effects are immediate and occur when a certain radiation threshold is exceeded, while stochastic effects are long-term, probabilistic risks that accumulate over time. For fetal exposure, deterministic effects, such as birth defects or growth restriction, are generally associated with much higher radiation doses than those typically received from diagnostic CT scans. Stochastic effects, primarily the increased risk of childhood cancer, are a theoretical concern even at low doses, but the absolute risk from a single, appropriately indicated bay car ct scan is considered very low.
Leading medical organizations, including the American College of Radiology (ACR) and the American College of Obstetricians and Gynecologists (ACOG), agree that the risk to the fetus from radiation exposure below 50 mGy is negligible. The radiation dose from most diagnostic imaging procedures used in trauma, including a standard bay car ct scan, falls well below this threshold. In fact, for scans that don’t directly include the fetus in the imaging field, like a head or chest CT, the fetal radiation exposure is often comparable to or even less than the background radiation received during pregnancy.
Table 1. Estimated Fetal Radiation Dose for Common Trauma Imaging Procedures
| Examinations Using Ionizing Radiation | Estimated Fetal Dose [mGy] |
|---|---|
| Radiography | |
| Cervical spine (AP, lateral) | |
| Extremities | |
| Chest (PA, lateral) | 0.002 |
| Thoracic spine | 0.003 |
| Lumbar spine (AP, lateral) | 1 |
| Pelvis | 1.2 |
| Computed Tomography (CT) | |
| CT Head | 0 |
| CT Chest | 0.2 |
| CT Abdomen | 4 |
| CT Abdomen and pelvis | 25 |
| CT Angiography aorta | 34 |
This table highlights that even a CT scan of the abdomen and pelvis, which directly images the fetal area, typically results in a fetal radiation dose significantly lower than the 50 mGy threshold. Therefore, when a bay car ct scan is medically necessary to assess injuries in a pregnant trauma patient, it should not be withheld due to unfounded fears of radiation. The risk of missing a life-threatening maternal injury far outweighs the minimal potential risk to the fetus from the radiation exposure.
Imaging Modalities in the Trauma Bay: From Initial Radiographs to Advanced CT Scans
In the trauma bay, the initial approach to imaging a pregnant woman injured in a car accident is similar to that for any trauma patient. The immediate priorities are to identify life-threatening injuries and guide resuscitation efforts. This often starts with radiographs and Focused Assessment with Sonography for Trauma (FAST) or extended FAST (e-FAST), before progressing to a bay car ct scan if indicated.
3.1. Radiography: The First Step in Trauma Assessment
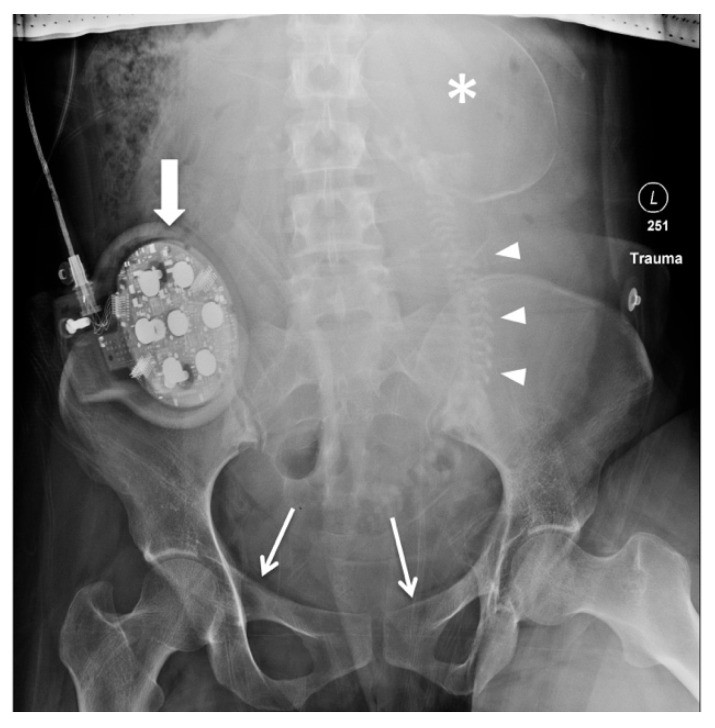
Radiographs, or X-rays, are typically the first imaging studies performed in the trauma bay. For a pregnant woman after a car accident, these usually include chest and pelvis X-rays, and potentially extremity X-rays depending on the clinical situation. Chest radiographs can quickly identify critical conditions like pneumothorax, hemothorax, or rib fractures. Pelvic radiographs, as shown in Figure 1, are particularly important as pelvic fractures in a pregnant woman after a car accident can indicate significant force to the uterus and potential placental or fetal injury. Pelvic fractures necessitate prompt obstetric evaluation, especially if the pregnancy is at a viable gestational age.
Figure 1. Pelvic Radiograph in Pregnant Trauma Patient
Pelvic radiograph of a pregnant patient at 28 weeks gestation after a car accident. Fractures of the pubic rami are visible. Note the fetal skeleton, including the skull and spine. This image demonstrates the need for careful assessment of pelvic injuries in pregnant trauma patients.
3.2. Computed Tomography (CT): The Cornerstone for Detailed Injury Evaluation
Computed Tomography (CT) has become an increasingly vital tool in trauma care, and its use in pregnant women, when indicated, is equally important. While radiography provides a general overview, a bay car ct scan offers detailed cross-sectional images of the body, allowing for the detection of a wide range of injuries with high accuracy. In the context of a car accident, a bay car ct scan can identify injuries to the brain, spine, chest, abdomen, and pelvis, including soft tissue and vascular injuries that are often missed by other imaging modalities.
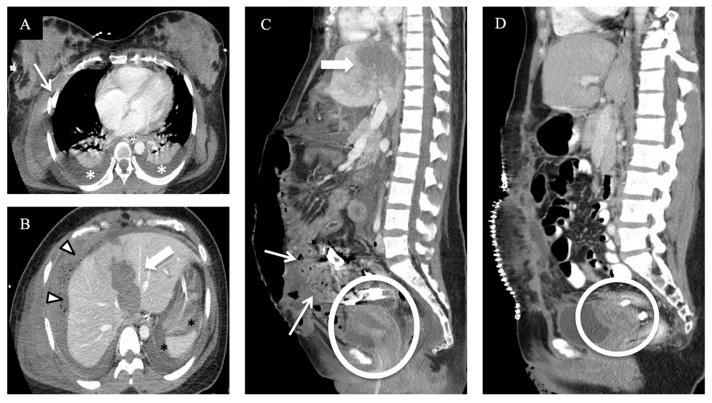
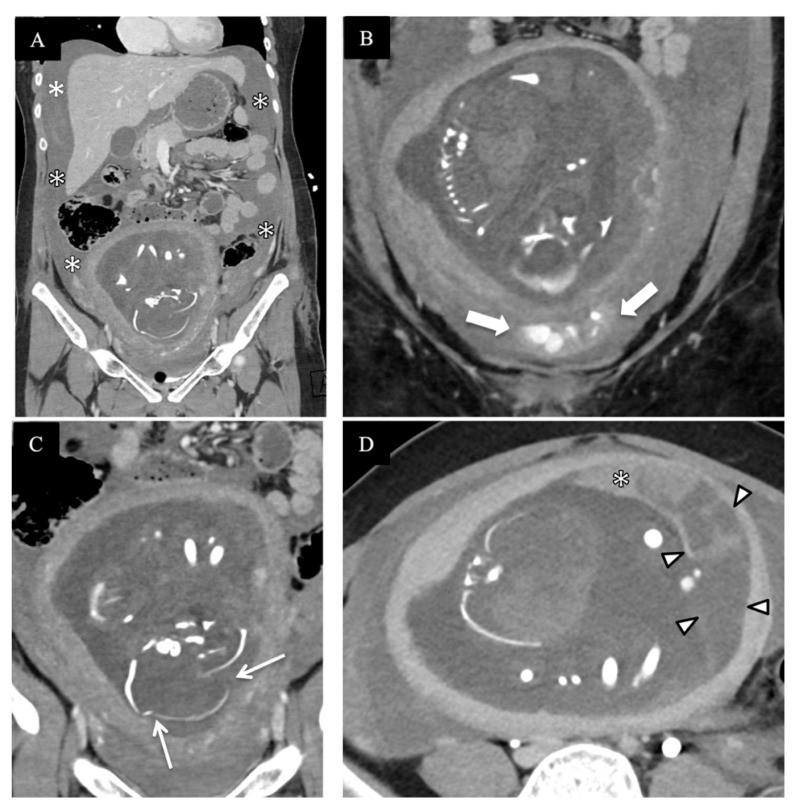
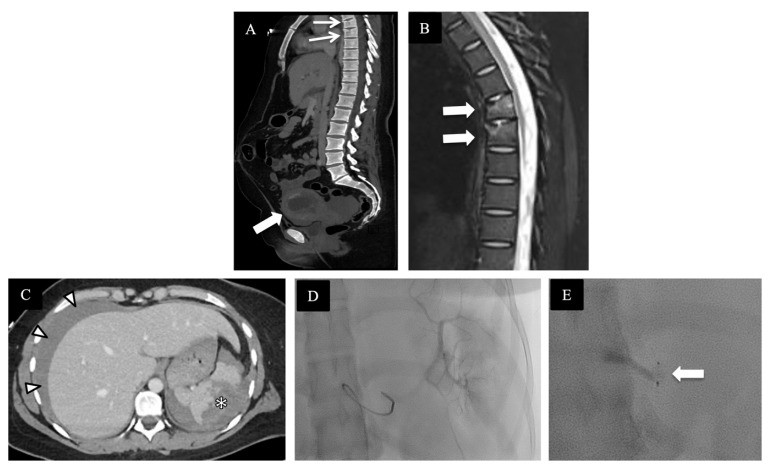
Standard trauma CT protocols, which are generally followed for pregnant patients as well, often include a non-contrast CT of the head and cervical spine, a contrast-enhanced CT of the chest, and a contrast-enhanced CT of the abdomen and pelvis. The use of intravenous contrast is crucial for visualizing vascular injuries and organ damage. As demonstrated in Figures 2, 3, 4, and 5, CT scans can reveal a spectrum of injuries in pregnant trauma patients, from liver lacerations and hemothorax (Figure 2) to complex spinal injuries and placental abruption (Figure 3), pelvic hemorrhage and fetal skull fractures (Figure 4), and splenic injuries (Figure 5).
Figure 2. CT Scan After Car Accident Showing Liver Laceration
CT images of a pregnant patient after a car accident revealing a severe liver laceration (Grade V) and other injuries. This case emphasizes the critical role of CT in identifying and characterizing complex abdominal trauma.
Figure 3. CT Scan Showing Spinal and Pelvic Injuries After High-Speed MVC
CT images demonstrating severe injuries in a pregnant patient involved in a high-speed car accident, including femoral fracture, occipital condyle fracture, and a hyperflexion-distraction injury of the thoracic spine, as well as placental abruption. This illustrates the comprehensive assessment possible with trauma CT.
Figure 4. CT Scan Revealing Pelvic Hemorrhage and Fetal Injuries
CT images showing active pelvic hemorrhage and fetal skull fractures in a pregnant patient after a high-speed car accident. This underscores the ability of CT to detect both maternal and fetal injuries in severe trauma.
Figure 5. CT and Fluoroscopy in Splenic Injury Management
CT and fluoroscopic images illustrating the diagnosis and management of splenic injury in a pregnant patient after a car accident. CT is crucial for initial diagnosis, while fluoroscopy guides interventional procedures like splenic artery embolization.
3.3. Ultrasound (FAST/eFAST): A Rapid and Radiation-Free Initial Assessment
Ultrasound, particularly the FAST exam, is a valuable tool in the trauma bay because it is portable, readily available, and does not use ionizing radiation. FAST is primarily used to detect free fluid in the abdomen (hemoperitoneum) and around the heart (hemopericardium), indicating internal bleeding. Extended FAST (e-FAST) also includes assessment for pneumothorax. While FAST is highly specific, its sensitivity for detecting intra-abdominal injuries, especially in pregnant women, is lower than CT. The altered anatomy of pregnancy can make sonographic assessment more challenging, and ultrasound is not as effective in visualizing retroperitoneal hemorrhage, solid organ injuries, or injuries to the bowel, mediastinum, aorta, or spine. Therefore, while FAST is a useful adjunct in the initial assessment, it is not a substitute for a bay car ct scan when detailed evaluation is needed.
3.4. MRI and Fluoroscopy: Limited Role in Initial Trauma Imaging
Magnetic Resonance Imaging (MRI) is generally not practical for the initial evaluation of pregnant trauma patients in the acute trauma bay setting. MRI scans take longer to perform and are less suitable for unstable patients requiring immediate interventions. However, MRI can be valuable in the secondary assessment of injuries after the patient is stabilized, particularly for evaluating spinal cord injuries, complex neurological issues, and soft tissue injuries, and for follow-up imaging to minimize radiation exposure.
Fluoroscopy, while essential for interventional radiology procedures like angiography and embolization to control bleeding, also involves ionizing radiation. The radiation doses in fluoroscopic procedures can be higher than diagnostic CT scans. Therefore, while life-saving in certain situations, fluoroscopy should be used judiciously, adhering to the ALARA principle (As Low As Reasonably Achievable) to minimize radiation exposure to both the mother and fetus.
Local Data: Experience with Bay Car CT Scans in Pregnant Trauma Patients
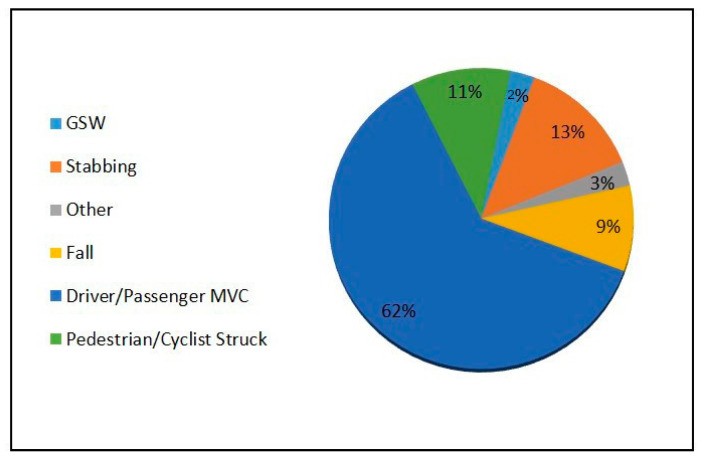
To further understand the clinical application of bay car ct scans in pregnant trauma patients, reviewing local data can be insightful. A retrospective review of pregnant patients presenting to a Level-1 Trauma Center over a 21-year period provides valuable real-world experience. During this time, 76 pregnant patients with major trauma were included in the trauma registry. Motor vehicle collisions were the leading cause of trauma in this cohort, as illustrated in Figure 6.
Figure 6. Mechanisms of Trauma in Pregnant Patients
This chart shows the distribution of trauma mechanisms in pregnant patients, highlighting motor vehicle collisions as the most frequent cause of injury, reinforcing the relevance of “bay car ct scan” scenarios.
In this study, a significant majority (81.5%) of pregnant trauma patients underwent CT examination as part of their initial assessment. Of those, a large proportion (67.7%) received whole-body trauma CT scans, including head, neck, chest, abdomen, pelvis, and spine imaging. This data underscores the reliance on CT scans, including bay car ct scans, in the comprehensive evaluation of pregnant women after major trauma. While radiation risks were discussed in some cases, and a few patients declined CT, the overwhelming majority received this crucial diagnostic imaging, highlighting its perceived benefit in these critical situations.
Conclusion: Bay Car CT Scans are Essential for Optimal Care in Pregnant Trauma Patients
Imaging trauma in pregnancy, especially in the context of car accidents requiring trauma bay management and potential bay car ct scans, presents unique challenges. While concerns about fetal radiation exposure are valid, it is crucial to recognize that withholding necessary CT scans due to these concerns can be detrimental to maternal and fetal outcomes. When indicated by the mechanism of injury, clinical findings, and initial assessments like FAST/e-FAST and radiographs, a bay car ct scan should be performed without hesitation, following established trauma protocols.
The rapid and accurate diagnosis of maternal injuries afforded by a bay car ct scan is paramount for achieving maternal stabilization, which is the most critical factor influencing fetal well-being after trauma. The radiation exposure from a single, well-justified bay car ct scan in the trauma setting is generally low and carries a negligible risk of significant fetal harm. In complex cases requiring multiple CT scans or fluoroscopic procedures, consultation with a medical physicist can help optimize imaging protocols and further minimize radiation exposure while ensuring optimal diagnostic accuracy. Ultimately, the judicious and appropriate use of bay car ct scans is an indispensable part of providing the best possible care for pregnant women who experience trauma, particularly in high-risk scenarios like car accidents.
Author Contributions
Conceptualization, F.H.B., and S.R.Q.; methodology, R.M., F.H.B. and S.R.Q.; validation, R.M. and S.R.Q.; formal analysis, R.M. and S.R.Q.; resources, A.P., F.H.B. and A.B.N.; data curation, R.M. and A.P. Writing—original draft preparation, R.M. and S.R.Q. Writing—review and editing, all authors: R.M., F.H.B., A.P., J.A.R., M.E.O., R.A.M., D.B.M., G.L., H.H., A.B.N. and S.R.Q.; visualization, R.M., F.H.B. and S.R.Q.; supervision, F.H.B. and S.R.Q.; project administration, S.R.Q. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.

