The urinary bladder, a vital organ in the human body, acts as a temporary reservoir for urine produced by the kidneys. With an average capacity ranging from 300 to 500 cc in adults, the bladder receives urine via the ureteric orifices and expels it through the urethral orifice during urination. Point-of-care ultrasound (POCUS) of the bladder has emerged as an invaluable tool for clinicians, offering rapid and non-invasive assessments directly at the patient’s bedside.
This guide delves into the applications, techniques, and interpretations of point-of-care bladder scans, equipping healthcare professionals with the knowledge to effectively utilize this modality for improved patient care.
Indications for Point-of-Care Bladder Scan
Point-of-care bladder ultrasound is indicated in a variety of clinical scenarios, providing crucial information for diagnosis and management. Key indications include:
- Bladder Volume Estimation: Accurate assessment of bladder volume is essential in managing urinary retention, monitoring fluid balance, and guiding catheterization decisions. POCUS provides a rapid and reliable method for volume estimation, particularly when compared to invasive catheterization.
- Detection of Bladder Mass: POCUS can effectively identify bladder masses, including potential tumors like transitional cell carcinoma. Early detection of bladder masses through POCUS can lead to timely referrals and interventions, improving patient outcomes.
- Evaluation of Bladder Outlet Obstruction (BOO): Suspected bladder outlet obstruction, often due to benign prostatic hyperplasia (BPH) in males or urethral strictures, can be readily assessed with POCUS. Increased post-void residual volume and bladder distention visualized on ultrasound can indicate BOO, prompting further investigation.
- Assessment of Hematuria: In patients presenting with hematuria (blood in urine), bladder POCUS can help rule out or identify potential bladder pathologies such as tumors, stones, or infections that may be the underlying cause.
- Investigation of Hydronephrosis: Hydronephrosis, or swelling of the kidney due to urine backup, can be secondary to bladder outlet obstruction or other urinary tract issues. Bladder POCUS can be part of the assessment to evaluate for distal obstruction as a cause of hydronephrosis.
- Evaluation of Anuria or Oliguria: In cases of anuria (no urine production) or oliguria (low urine production), bladder POCUS can quickly determine if the bladder is empty or contains urine. An empty bladder in these scenarios may suggest pre-renal or renal issues, while a full bladder could indicate urinary retention.
- Diagnosis of Flank or Pelvic Pain: Patients presenting with unexplained flank or pelvic pain may benefit from bladder POCUS to evaluate for bladder distention, stones, or other bladder abnormalities that could be contributing to their symptoms.
- Confirmation of Foley Catheter Placement: After Foley catheter insertion, POCUS can be used to confirm proper placement within the bladder and ensure inflation of the catheter balloon within the bladder cavity, preventing urethral injury.
Performing a Point-of-Care Bladder Scan
Performing a bladder POCUS is a straightforward procedure. Here are the key steps:
-
Transducer Selection: A low-frequency curvilinear transducer is typically ideal for bladder scanning due to its penetration depth and wider field of view, which is necessary to visualize the entire bladder. If a curvilinear transducer is unavailable, a phased array low-frequency transducer can be used as an alternative.
-
Patient Positioning: Position the patient in a supine position to allow for optimal access to the bladder area.
-
Scanning Technique:
- Longitudinal View: Place the transducer midline on the abdomen, just superior to the pubic symphysis. Orient the transducer marker towards the patient’s head. Sweep cephalad and caudad to visualize the bladder in its long axis.
- Transverse View: Rotate the transducer 90 degrees clockwise, so the transducer marker is pointing towards the patient’s right side. Sweep from the pubic symphysis superiorly to visualize the bladder in its short axis.
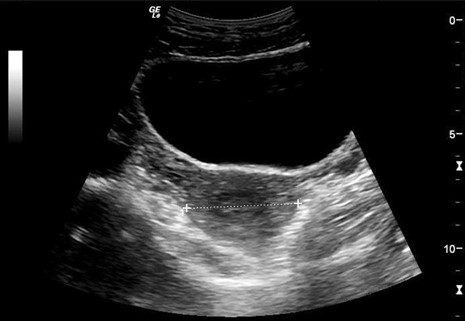
Figure 1. Transverse view of the urinary bladder, demonstrating its anatomical relation to surrounding pelvic structures. Note the uterus positioned posteriorly, highlighting the acoustic window provided by a full bladder for pelvic organ visualization.
A distended bladder serves as an excellent acoustic window, allowing for visualization of not only the bladder itself but also adjacent pelvic organs such as the uterus in females and the prostate in males.
- Bladder Volume Calculation: Bladder volume can be estimated using the ultrasound measurements. The ellipse method is commonly used:
- Obtain longitudinal and transverse views of the bladder.
- Measure the anteroposterior (AP), transverse (TR), and height (H) dimensions of the bladder in centimeters.
- Calculate the volume using the formula: Volume (cc) = AP (cm) x TR (cm) x H (cm) x 0.532 (correction factor).
- Many modern ultrasound machines offer automated bladder volume calculation, simplifying the process.
Figure 2. Bladder volume calculation using the ellipse method. This illustration details the standard measurements required for estimating bladder volume using the three-dimensional method in point-of-care ultrasound.
Common Findings on Point-of-Care Bladder Scan
Besides volume assessment, POCUS can reveal various bladder pathologies:
- Bladder Mass: Bladder masses, often indicative of tumors like transitional cell carcinoma, may be visualized as irregular, solid masses projecting into the bladder lumen. POCUS can detect these masses, even in asymptomatic patients, prompting further diagnostic workup such as cystoscopy.
Figure 3. Ultrasound image showing a bladder mass. This image demonstrates a typical presentation of a bladder mass identified during a point-of-care ultrasound examination, necessitating further oncological assessment.
- Bladder Diverticulum: Bladder diverticula are outpouchings of the bladder wall. They are often incidental findings on ultrasound and may contain urine or, rarely, stones. POCUS can identify diverticula and sometimes visualize the neck connecting the diverticulum to the bladder.
Figure 4. Point-of-care ultrasound image revealing a small bladder diverticulum. The image clearly shows a small, pouch-like protrusion from the bladder wall, characteristic of a bladder diverticulum.
- Bladder Stones (Calculi): Bladder stones appear as echogenic foci within the bladder lumen, often with posterior acoustic shadowing. A key characteristic of bladder stones is their mobility. To assess mobility, patients can be rolled into the lateral decubitus position (left or right side). Mobile stones will shift position within the bladder, whereas impacted stones at the ureterovesical junction will remain stationary.
Figure 5. Ultrasound image of a single bladder calculus. This image highlights a solitary echogenic bladder stone, a common finding that point-of-care ultrasound can quickly identify.
Figure 6. Demonstrating bladder calculus mobility with patient repositioning. This sequential imaging shows a bladder stone shifting position when the patient was rolled onto their right side, confirming the stone’s mobility within the bladder.
Conclusion
Point-of-care bladder ultrasound is a rapid, non-invasive, and highly valuable diagnostic tool for clinicians across various medical specialties. Integrating bladder POCUS into clinical practice enhances diagnostic accuracy and efficiency in numerous scenarios, from assessing urinary retention to identifying bladder pathologies. Remember to always correlate POCUS findings with the patient’s clinical history for comprehensive patient evaluation.
Beyond the findings discussed, POCUS can also assess for ureteric jets using color or power Doppler, indicating ureteral patency and helping to identify potential urinary obstructions. In elderly males, bladder POCUS can incidentally reveal signs of benign prostatic hyperplasia (BPH) and bladder outlet obstruction, enabling early intervention and preventing potential kidney damage. By incorporating point-of-care bladder ultrasound, clinicians can significantly improve patient care and outcomes in a wide range of clinical settings.
Enhance your expertise in renal POCUS with the POCUS Renal/Genitourinary Certificate.
References
AIUM Practice Parameter for the Performance of an Ultrasound Examination in the Practice of Urology. (2011). The American Institute of Ultrasound in Medicine. https://www.aium.org/resources/guidelines/urology.pdf
Southgate, S. & Herbst, M. (2001). Ultrasound of the Urinary Tract. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK535381/